Contents
Introduction
- About Confident Teen
- Key Components and Organizational Commitments
- Purpose of Confident Teen
- Program Needs and Significance
- Importance of Confidentiality
- Importance of Adolescent-Friendly Environments
- 4 Cs of Confident Teen
- Section in Review
Preparing Organizations to Implement
Coordination
Collaboration
- Establish a Network of Adolescent-Friendly Partners
- Tips for Referral Best Practices
- Additional Resources for Adolescents
- Section in Review
Communication
- Information for Providers
- Talking with Adolescent Patients
- Tips for Talking with Adolescent Patients
- Sample Conversations for Providers
- Discussing Sensitive Topics
- Section in Review
Care
Introduction
About Confident Teen
The Confident Teen program contains an organizational policy that provides adolescent patients (ages 12 and older) private time with providers during all primary care visits to ask questions and talk about health concerns. Confident Teen provides a stepping stone for privacy, fosters independence for teens, allows adolescents the opportunity to advocate for their own health and builds skills for navigating and engaging in the healthcare system. At the organizational level, Confident Teen provides a supportive environment that optimizes the healthcare experience for all adolescent patients. This toolkit contains support resources and all information needed for healthcare organizations to successfully implement the Confident Teen program.
Development Process
Confident Teen was developed through the Comprehensive Healthcare for Adolescents Initiative (CHAI) project from Fall 2020 through Summer 2021. The CHAI project team worked with six organizational partners and a teen advisory group (TAG) to gather insights on the healthcare experience for adolescents. Using a human-centered, sixstage design process, a network of subject-matter experts (SMEs) used insights to gain a deeper understanding of root problems faced by adolescents and brainstormed innovative solutions. One of those solutions is Confident Teen. Network partners represented a variety of context expertise to contribute their knowledge and experience to this process, while the TAG provided continuous feedback throughout the design process.
Key Components and Organizational Commitments
By implementing this program, your organization will provide adolescents with quality, individually-tailored healthcare. This includes providing adequate one-on-one time between adolescent patients and providers to address questions or concerns while ensuring confidentiality. To build trust and promote transparency, it is important to communicate the clinic’s confidentiality policy and accompanying procedures to patients, their parents/guardians, and other relevant stakeholders. To support and enable confidential conversations, it is essential to create adolescent-friendly environments, ensure staff and providers embody adolescent-friendly characteristics, and provide accessible resources for patients.
Purpose of Confident Teen
Confident Teen uses a clinic policy to ensure adolescent patients have one-on-one time with their healthcare provider, discuss confidentiality between a patient and provider, and address sensitive topics at the adolescents’ request. The goals of Confident Teen are:
- To improve adolescent experiences in healthcare settings.
- To improve adolescent access to sexual and reproductive health and mental health services in primary care settings.
Program Needs and Significance
Adolescence is a unique period in development when young people are able to make decisions about their health, but are still under a guardian’s care. Adolescent patients, even as minors, have a legal right to confidentiality and access specific medical services without parental consent or notification. Concerns about confidentiality can be a critical barrier for young people in seeking and receiving appropriate medical services. As stated by Riley et al (2015), “Adolescents may choose to forego medical care if they are concerned about confidentiality, hence physicians are missing opportunities to provide age appropriate and legally protected care to minor patients for sensitive medical and psychosocial issues.”
Adolescents’ trust in providers is a precondition to discussing sensitive topics. The literature suggests adolescents assured of confidentiality by a health care provider, are more willing to disclose sensitive information like substance use, mental health, and sexual history, compared to those for whom confidentiality was not mentioned. Maintaining confidentiality for adolescent patients receiving health services is an important aspect of ethical clinical practice. Maintaining confidentiality is an evidence-based component of quality care, and a key component of Patients’ Bill of Rights.
Policies and procedures related to confidentiality, along with an environment conducive to discussing sensitive information, are foundations to adolescent-friendly care.
Importance of Confidentiality
A major barrier to adolescents seeking health services is perceived lack of confidentiality. Providers may be unfamiliar with laws and policies regulating confidential care for minors. As a result, they may overcompensate by including parents/guardians in all aspects of the adolescent’s care, even when it inhibits services. Previous studies have found that without confidentiality, adolescents are less willing to discuss healthcare concerns with their provider, potentially skipping care altogether. Empirical data suggest adolescents forgo healthcare when confidentiality is not guaranteed, indicating confidentiality is a key factor in adolescents’ healthcare utilization. By ensuring information disclosed by adolescents to their providers is confidential, providers can enhance trust, satisfaction, adherence, and likelihood to return for continued services.
"The American Academy of Pediatrics (AAP) recommends that adolescent visits include 'private time' with providers to discuss sensitive issues and review confidential health screens (Society for Adolescent Health and Medicine, 2016, p.374)."
Confidentiality should be upheld, except in instances that warrant mandatory reporting and child protection concerns, specifically if the safety of a patient or others is at risk. Organizations should ensure all staff know the steps for reporting such cases to appropriate authorities, as required by law.
As stated by the American Medical Association (AMA):
When disclosing patients’ personal health information, physicians should:
- Restrict disclosure to the minimum necessary information; and
- Notify the patient of the disclosure, when feasible.
Physicians may disclose personal health information without the specific consent of the patient (or authorized surrogate when the patient lacks decision-making capacity):
- To other health care personnel for purposes of providing care or for health care operations; or
- To appropriate authorities when disclosure is required by law.
- To other third parties situated to mitigate the threat when in the physician’s judgment there is a reasonable probability that:
- The patient will seriously harm him/herself.
- The patient will inflict serious physical harm on an identifiable individual or individuals.
For any other disclosures, physicians should obtain the consent of the patient (or authorized surrogate) before disclosing personal health information.
Important of Policy
Confidentiality of adolescent patients often breaks down because there is no established policy regulating the processes to ensure confidentiality is provided. Policies provide guidance, consistency, accountability, efficiency, and clarity on how an organization operates. Confidentiality policies can improve healthcare experiences for adolescent patients, as well as dramatically improve their access to care.
Confidentiality policies and procedures are influenced by law and practice at both national and state levels. However, healthcare organizations can set internal policies, procedures, and practices that impact the type of care adolescent patients receive. For example, internal changes may include additional training for staff and providers, revising consent forms, and including useful electronic medical record features that broaden confidentiality protection for minors. These changes help build trust with patients and their parents/guardians, which contributes to confidence and comfort in the healthcare setting.
As stated by Pasternak et al (2019), “It is the position of the Society for Adolescent Health and Medicine (SAHM), the American Academy of Pediatrics (AAP), and the American College of Obstetricians and Gynecologists (ACOG) that policies should be developed to not impede the provision of confidential healthcare to adolescent patients.”
Importance of Adolescent-Friendly Environments
Creating an adolescent-friendly environment is important in ensuring a comfortable and safe space for adolescents. Pediatric clinics cater to young children (10 and under) and family medicine practices commonly cater to older adults. Adolescents (teens) may feel too old for pediatric environments while feeling apprehensive of or intimidated by adult clinics. This perception can often contribute to healthcare visits being a stressful experience for adolescents.
As a result, organizations have opportunities to address the unique needs of adolescents. Various strategies exist to create healthcare settings that support and enable adolescents to feel confident communicating their health needs, including but not limited to:
- PHYSICAL SPACE. Creating waiting areas that represent local, teen culture contributes to adolescents’ comfort and decreases patient anxiety.
- PERSONNEL. Staff who are welcoming and accommodating facilitate adolescent engagement with the organization. Particularly, young people connect better with staff perceived as friendly, relatable, and culturally understanding.
- PROCESS. Leveraging novel resources, such as technology, provides adolescents with an opportunity to connect with their care team out-of-office. Patients can stay engaged in their healthcare by expressing concerns and as they arise, access health records, and learn about health promotion through texting, apps, patient portals, and e-messaging.
Strategies that create a welcoming environment and connection to providers above have been identified as key constructs in establishing adolescent-friendly care. These domains align with the World Health Organization (WHO) framework of adolescent-friendly health care, as well as with principles of patient-centered care.
4 "C"s of Confident Teen
Just as Confident Teen was developed using a human-centered design process and approach, it must be implemented in a patient-centered manner to help ensure successful outcomes. Patient-centered care (PCC) is a key element of high-quality care centered on the qualities of personal, professional, and organizational relationships. PCC is an approach to care that focuses on the patient rather than an illness or diagnosis. In addition, PCC encourages patients to actively engage in their own care while emphasizing communication, partnerships, and health promotion in the provider-patient consultation. PCC is associated with improved health outcomes, positive health-seeking behaviors, patient satisfaction, and improved health service utilization.
Similar to PCC, adolescent-friendly care is a theoretical framework for improving the quality of care. However, adolescent-friendly care focuses on quality service delivery for young people. Key domains of the adolescent-friendly care framework include healthcare accessibility, staff attitudes, communication, evidence-based guideline-driven care, age-appropriate environments, healthcare involvement, and health outcomes. Webb et al. (2017) report PCC and adolescent-friendly care frameworks provide a strong theoretical basis to meet the health care needs of adolescents. These theoretical frameworks help guide what is defined as the 4 Cs of adolescent patient-centered care: Coordination, Collaboration, Communication, and Care.
The contents of this toolkit are organized by using the 4 Cs approach. Each of the 4 Cs are composed of organizational, interpersonal, and individual level elements to be addressed. An overview of each component is given below.
- Coordination: The process and practices that must occur among organizational leadership and administrators to ensure Confident Teen can be implemented effectively and efficiently to meet the needs of adolescent patients.
- Collaboration: The need to utilize an interdisciplinary approach to ensure adolescent healthcare needs are met and facilitating referrals and warm hand-offs to other adolescent-friendly providers as needed.
- Communication: The interpersonal communication between providers and patients, which includes the verbal and nonverbal actions to support adolescents in their healthcare experience.
- Care: The process of ensuring confidential care is provided to adolescent patients to meet their needs and help them learn to navigate the healthcare system independently.
Section in Review
SRH and MH needs often go unmet and form a complex web of potential challenges to adolescent development. Implementing Confident Teen presents an opportunity to embed SRH and MH into primary care visits. The following list summarizes key information about the background and significance of Total Teen:
- Confident Teen screens adolescent patients (ages 12 and up) for SRH and MH needs during primary care visits and prompts micro visits, referrals, and follow-up services based on results.
- Confident Teen incorporates adolescent-friendly processes (a screening questionnaire, confidential follow-up discussions, and comfortable environments) to improve access to and experiences with healthcare.
- These processes foster independence for teens, build skills for navigating and engaging in the healthcare system, and allow adolescents the opportunity to advocate for their own SRH and MH.
- Organizations must implement Confident Teen in an adolescent patient-centered manner to help ensure successful outcomes.
The next section, Preparing Organizations to Implement, discusses steps to create an adolescent-friendly environment that supports and enables implementation of Confident Teen.
Preparing Organizations to Implement
Program Orientation
Confident Teen includes a mandatory program orientation that will prepare your organization for implementation. The program orientation includes various components (both online/asynchronous, and in-person) to ensure your team is prepared to implement Confident Teen successfully, and identifies opportunities to pursue professional development as needed. The in-person component of the program orientation will serve as a time for members of the CHAI team to work through key components of CT with members of your team. To ensure this time is as productive as possible, we strongly recommend organizations include the following people from your team:
- Site Champion (one person that is the “go-to” for CHAI programs at your
organization) - Front desk staff / Patient services representative (someone that interacts with
patients in non-medical care role (e.g. receptionist, etc.)) - Clinician / Provider (a care provider)
- Organization representative (a decision-maker regarding policies and procedures,
etc.)
Adolescent-Friendly Environments
The clinic environment plays a major role in adolescents’ experiences with healthcare services. Therefore, the physical clinic environment should facilitate open communication between adolescent patients and the healthcare team. This section provides resources for the clinic team to ensure their environment is comfortable, accepting, and welcoming of adolescents from all walks of life.
Clinic Assessment
The first step in ensuring your clinic is adolescent-friendly is to complete a clinic assessment. The first two tools listed below are comprehensive assessments focused on various factors related to adolescent-friendly healthcare, while the third tool will help the team focus on the physical environment.
1. Youth-Led Health Center Assessment Tool
Source: Adolescent Health Initiative
This resource will link you to an assessment tool, a facilitator guide, and accompanying video with adolescents reflecting on what is important to them when accessing health care services. This tool is intended to be completed by a small group of adolescents, so your organization can experience the first-person point of view of at least three teens to find out what they notice while waiting for their appointments.
Click here to download the Youth-Lead Health Center Assessment Tool.
2. Youth-Friendly Services Assessment Tool & Guide
Source: Healthy Teen Network
This resource is an interactive tool, including a guide and complete bibliography, which helps assess if your clinic delivers services in a youth-friendly manner. The tool is comprehensive with a focus on service-delivery as well as the clinic environment.
Click here to access the Youth-Friendly Services Assessment Tool and Guide.
3. Physical Environment Assessment Tool
Source: The CHAI Project at Texas A&M University
This tool will help you assess various aspects of the physical environment of your clinic space. Through this instrument you will analyze the large-scale environment, down to small-scale details and accessories that contribute to the look and feel of your clinic space. A copy of the tool is provided at the end of this section.
These tools can assist your organization in identifying gaps and areas for improvement. Specific tactics are described in the sections below to guide you in modifying your clinic environment (i.e., both large and small-scale environments).
Click here to download the Physical Environment Assessment Tool.
Large-Scale Environmental Considerations
Entering a healthcare facility can be nerve-wracking — from large, crowded, public spaces to information-rich, sterile exam rooms. Adolescents can experience multiple spaces and settings within the larger facilities during a single appointment. Fortunately, healthcare organizations can leverage the design of these spaces to promote comfortable, equitable, and engaging areas for adolescents to feel comfortable and ready to approach their appointment.
The concepts below are briefly explained for contextual purposes. Organizations are encouraged to utilize the included Physical Environment Assessment Tool to explore how their organization approaches these concepts.
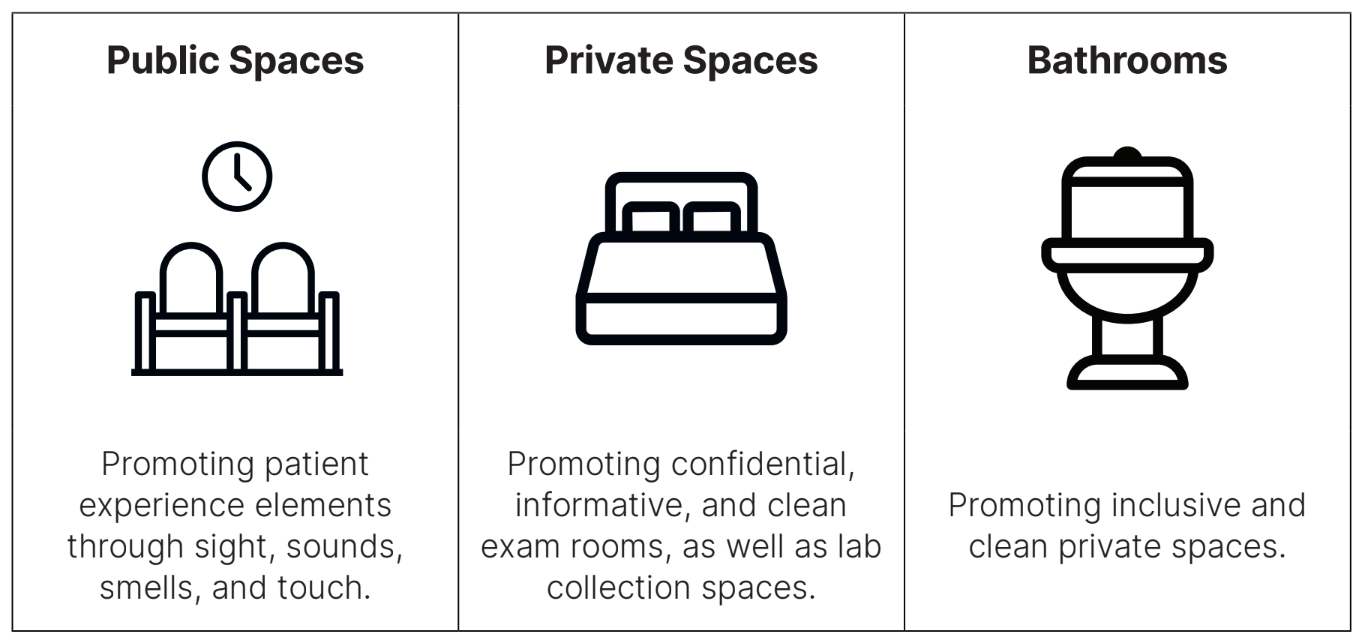
Design Considerations
Public Spaces can be overwhelming and lead to “information-overload”, so avoid having too many text-heavy posters or postings. These spaces can also be off-putting in design, making adolescents feel out of place. Feature decor that does not cater to one particular age group or demographic. Instead, try to have welcoming decor that is inviting to all groups and demographics.
Private Spaces, especially small spaces, can quickly become cluttered. Be careful to not over-decorate with information-rich content. Too much information can be overwhelming and the clutter may increase patient anxiety.
Bathrooms are opportunities to provide hidden services such as anonymous question submission, and advertisements for local programs or resources. Some clinics have even created a sample labeling system for patients to confidentially notify providers they are in a dangerous situation (e.g., providing patients with black and red sharpies to self-label urine samples; the red sharpie was to be used if the patient was experiencing violence or danger at home). If tear cards that advertise services are provided, be sure to tear the first two-three cards away from the display so the adolescent isn’t reluctant to be the “first” to remove an information tear card.
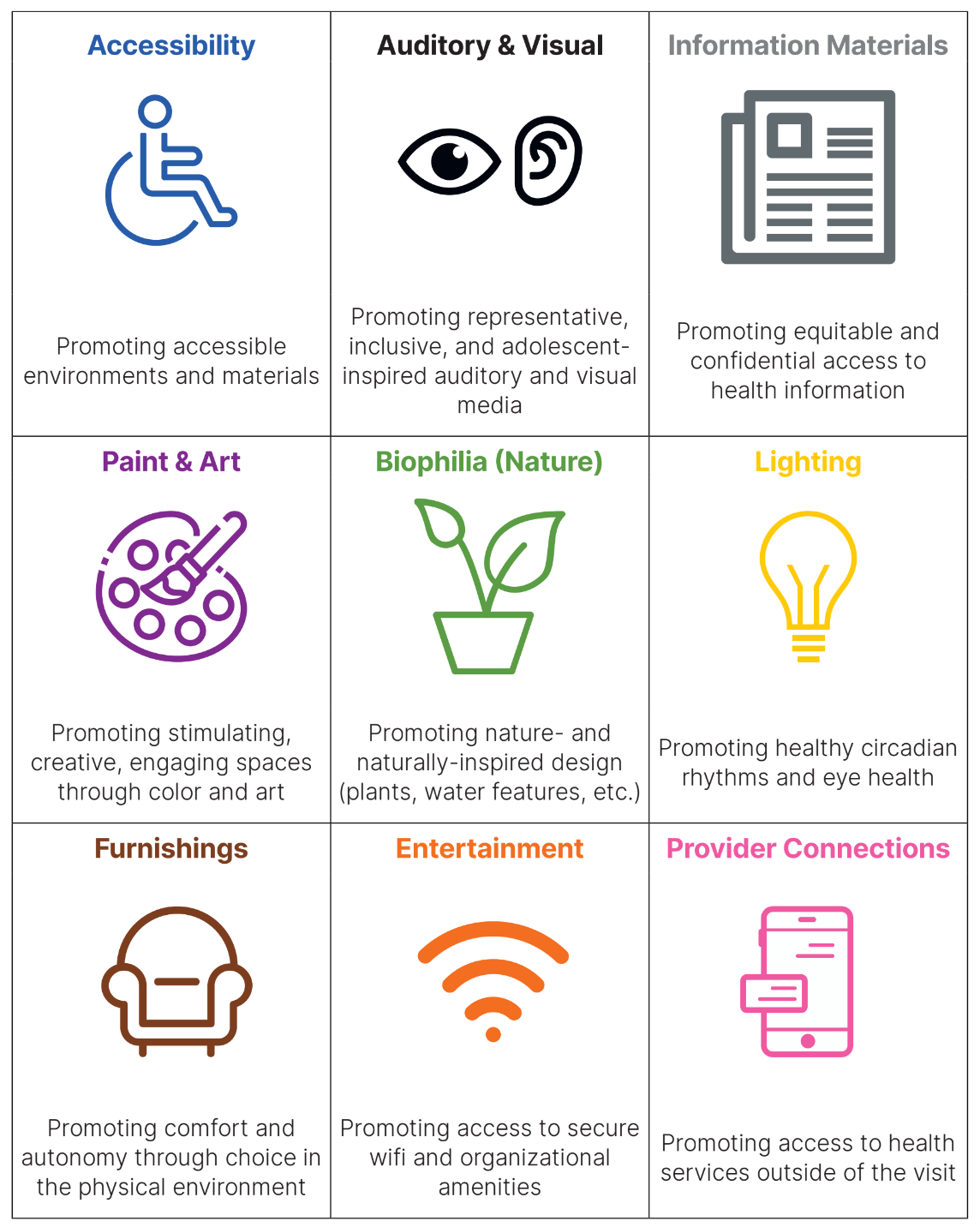
Small-Scale Environmental Considerations
Experiences and perceptions of a space can vary greatly depending on a person’s race, ethnicity, sexual orientation, gender identity, age, ability level, income, and other factors. While this is not an exhaustive list, it is meant to provide examples of areas to address in order to enhance the adolescent’s clinic experience.
Informational Posters
Click here to download a PDF of sample posters.
Technology Requirements
Your organization will make the Confident Teen Assessment accessible to adolescents via a tablet or iPad. It is recommended your organization have at least two tablets for the Confident Teen Assessment to accommodate for patient caseload and the number of providers seeing patients simultaneously.
When setting up the assessment on tablets, adjust the screen lock/sleep settings so the device does not lock out adolescents. A lockdown screen can be used to limit distractions and access to other apps while completing the assessment. Organizations can also add adolescent friendly websites to the tablets for patients to browse while waiting to see their provider (see the Communication section for a list of health resources for teens).
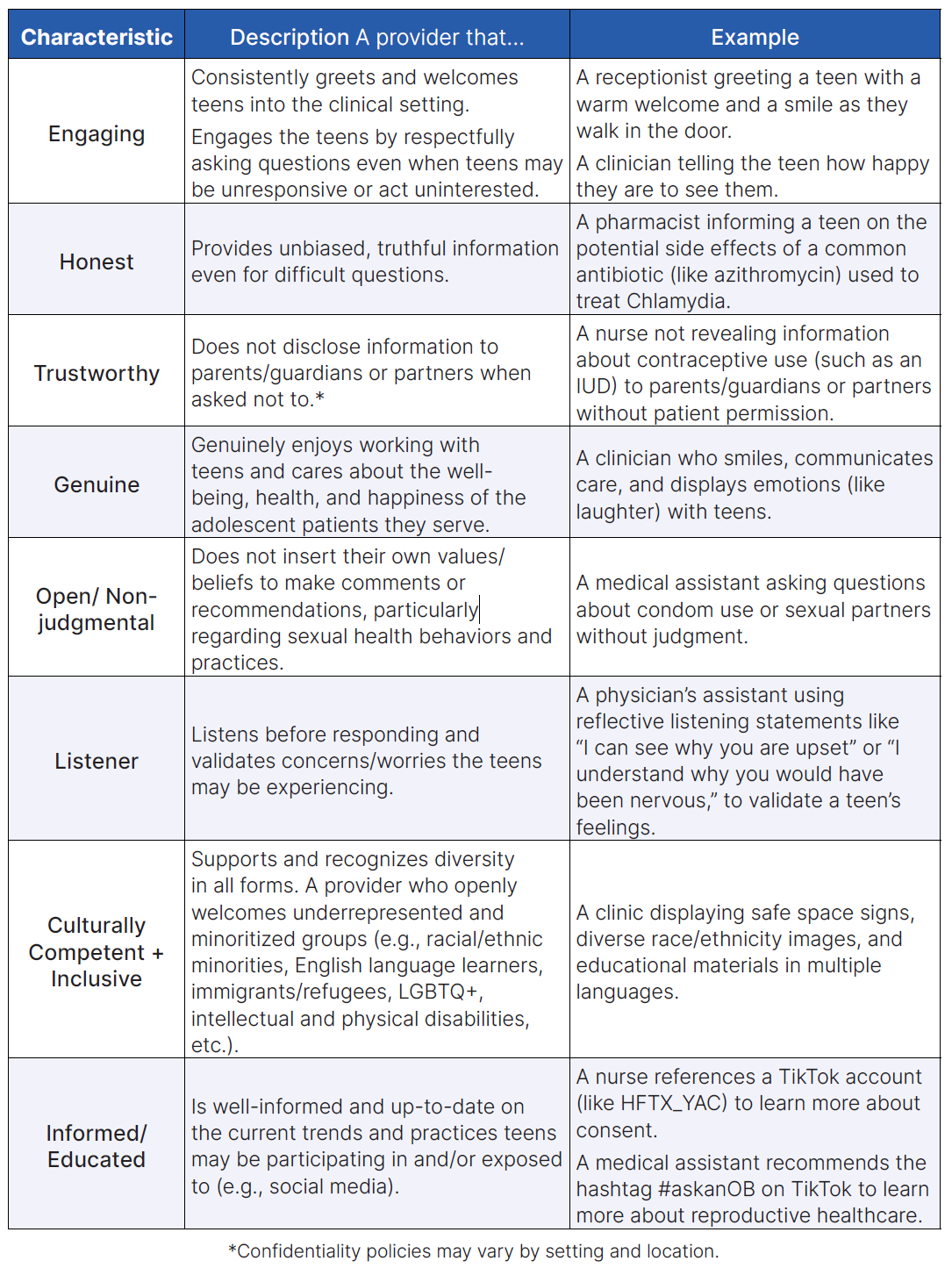
Adolescent-Friendly Providers and Staff
Adolescent friendly environments do not stop at the physical space; they are also impacted by the staff and providers within the facility. Clinics providing services to adolescents should ensure their staff and providers demonstrate adolescent-friendly characteristics (see table below). It is often the receptionist at check-in who sets the tone for the entire visit.
Adolescent-friendly providers are uniquely qualified to provide services in a way to further empower teens to take ownership over their health and healthcare experience. Provider-level approaches are used to help adolescents, their families, and friends to feel welcome, comfortable, accepted, and safe. This includes the personality traits and characteristics, and interpersonal tactics of providers (e.g., clinicians, physicians, nurses, receptionists, pharmacists, etc.), which equip them to work competently and sensitively with adolescents.
Characteristics of Adolescent-Friendly Providers
Below are characteristics of adolescent-friendly providers and staff, along with examples of those characteristics in action.
Provider Self-Assessment
All staff in your organization should complete a self-assessment to assess their respective competency in the characteristics of adolescent-friendly service delivery. The tools listed below are recommended and will also identify potential opportunities for professional development and changes in your service delivery approach. All staff who are a point of contact with adolescents should complete the assessment, not just medical providers.
“Giving providers a direct role in their own assessment could enhance the effectiveness of supervisory visits because the provider has already considered his or her performance and assessed its strengths and weaknesses. Self-assessment also has the potential to reinforce medical standards and to increase worker accountability” (USAID).
1. Adolescent-Friendly Provider Self-Assessment Tool
Source: The CHAI Project at Texas A&M University
The Adolescent-Friendly Provider Self-Assessment tool was derived using compelling questions from existing, more comprehensive assessment tools from the International Planned Parenthood Federation (2008) and Engender Health (2002). This tool is intended to serve as a starting place for self-assessing adolescent-friendly practices among staff and providers, and identify areas of opportunity for professional growth and development. To learn more about these assessments, these sources are included in the References section at the end of this manual.
Click here to download the Adolescent-Friendly Provider Self-Assessment Tool.
2. Youth-Friendly Services Assessment Tool
Source: Healthy Teen Network
The Healthy Teen Network Youth-Friendly Services Assessment Tool is an interactive tool, including a guide and complete bibliography, to help assess if your clinic delivers services in a youth-friendly manner. Though this tool was listed previously as a clinic assessment, it is listed here again because it includes sections on staff and provider-level approaches.
Click here to download the Youth-Friendly Services Assessment Tool.
3. Being Youth-Friendly
Source: The University of Michigan Adolescent Health Initiative (AHI)
The University of Michigan Adolescent Health Initiative has a tool within their Spark program titled “Being Youth-Friendly.” This tool introduces “elements of an adolescent-centered environment and outlines key staff and provider behaviors that are essential to providing youth-friendly care.” The University of Michigan also has other Spark initiatives to assist providers and staff with training for adolescent patient-centered care.
Click here to download the Being Youth-Friendly Tool.
Adolescent-Friendly Provider Trainings
Adolescent patient-centered care requires continual efforts by staff and providers to ensure they are meeting the needs of their patients and providing quality confidential care. Total Teen entails organizational practices to assist your organization in providing services, but is not all-encompassing of the training and resources needed. Additional training and professional development should be considered based on opportunities for growth and improvement identified through clinic- and self-assessments. The training listed below is recommended by the CHAI team as a starting place when considering new ways to provide services and further develop staff and providers’ skill sets.
- Motivational interviewing and coaching
- Contraceptive counseling
- Mental health first aid
- Trauma-informed care
- Youth diversity, equity, and inclusion
- Conditional confidentiality
- Adolescent-patient-centered care youth to provider dialogues
Section in Review
The clinic environment, including both physical space and social climate, influences patient experiences. This section focused on creating an adolescent-friendly environment to aid Total Teen implementation. The following list summarizes key information and tasks from this section:
- Clinic spaces are an important factor in adolescent patients’ healthcare experiences. Organizations should determine whether a clinic is adolescent-friendly by completing clinic assessments.
- After completing a clinic assessment, organizations should identify ways to make their clinic spaces more adolescent-friendly using built structures, interior factors, and accessories.
- All clinic staff should periodically assess their respective competency in adolescent patient-centered care using validated tools and identify opportunities for professional development and improvements in service delivery.
The next section, Coordination, will focus on administrative practices essential to successful implementation of Confident Teen.
Coordination
The first pillar of adolescent patient-centered care for Confident Teen is coordination, which includes the process and practices that must occur among organizational leadership and administrators to ensure Confident Teen is implemented effectively. Coordination entails executing administrative practices that will enable healthcare organizations to implement the Confident Teen Policy. See the graphic below for Key Components of Coordination; these steps are further described in this section.
The Confident Teen Policy
When implementing Confident Teen, your organization will adopt a new clinic policy or modify existing policies and build mechanisms to carry out accompanying supportive activities in clinical services. The model policy (provided at the end of this section) should state your organization will provide adolescent patients one-on-one time with providers to discuss confidentiality between patients and providers. This time will also give the adolescent patients a chance to discuss any confidential questions or concerns they have regarding their health. The following text will discuss policy modification, adoption, and monitoring processes.
Model Policy
To adopt the Confident Teen Policy, your organization should incorporate new language into existing policies and procedures. A Policy and Procedures template and example are provided at the end of this section. Use these documents to develop organization-specific procedures. If needed, consult with your legal department/board to ensure the policy and procedures are permissible.
Policy Modification
The following items are recommendations and tips for modifying the policy and
procedures to best fit your organization.
- Review existing policies within your organization related to adolescent patients, privacy, and confidentiality.
- Talk with key stakeholders (i.e., those who will be subject to policy requirements, adolescents, parents/guardians, and those who will enforce policy adherence) to determine if policy modifications are necessary.
- Consult experts for advice. Legal experts can help ensure the policy modifications comply with state and federal regulations. Human resources professionals can address potential employee relations issues that may ensue as a result of this policy change.
- As your organization modifies the policy, ensure its wording, length, and complexity are appropriate for those who will need to endorse and implement it.
Policy Adoption and Institutionalization
Policy adoption and institutionalization should be done in a manner that fits your organization. By institutionalizing policies and practices, your organization can ensure consistency, stability, and durability.
Organizations should begin preparing for policy adoption as soon as possible. Based on your type of organization, different preparation processes are needed to set the stage for adoption.
Determine which, if any, of the following steps will help facilitate policy adoption at your organization:
- Holding an informational meeting about the policy with leadership
- Obtaining approval from the board of directors
- Setting an agenda item for publicly accessible meetings
- Regardless of the approval process required at your organization, ensure you have enough time for stakeholder leadership to review and endorse the policy.
Build Program Support
The Confident Teen Policy is most effective if those affected are consulted, supportive, and have the opportunity to consider and discuss the implications of the new procedures.
Begin building support prior to implementation and continue to build support during implementation. Additionally, program support should continue as part of continuous quality improvement once the policy and procedures are active.
Host a Listening Session
To begin building support for this policy, we recommend hosting a listening session with staff from different departments in your organization, so you can discuss the new approach and to take into account their perspectives and suggestions.
Depending on the type of healthcare organization, consider including:
- Clinic providers and staff
- Organization administration
- Board members
- Volunteers
- Adolescents or potential service users
- Parents/Guardians of adolescents
Use the steps below to guide your listening session to build program support:
- Describe the new proposed policy and discuss how it could impact staff.
- Be clear about the proposed timeline, specifically when and how you expect the policy to be incorporated into daily practice.
- Discuss benefits of the policy, as well as potential challenges.
- Develop a feedback system for staff who are unable to attend listening sessions in order to incorporate their input.
- Establish a plan for reporting barriers to implementation and reviewing policy progress, so changes can be made based on lessons learned.
Not all clinic staff will be able (or want) to attend the listening session regarding the Confident Teen Policy. You can ask staff who attend listening sessions to build internal support for the policy by encouraging them to share what they learned and how they anticipate the policy will impact their day-to-day work.
Communication with Staff
Communication about the new policy is necessary to ensure everyone within your organization is knowledgeable about the new policy and procedures. All staff should be informed about the policy, its purpose, and how the policy is to be implemented. Communication with clinic staff may occur via email, memos, or individual, small-group, or all-employee meetings. If using email or a memo, we recommend the following to ensure communications are distinguishable from routine communications your staff may overlook:
- Specify the topic in the subject line
- Mark the message as high importance
- Enable read receipts
When communicating about the policy, you should distribute a copy of the Policy and Procedures to all staff and include:
- The policy’s effective date
- A notice stating where the policy can be accessed (e.g. the employee handbook or the organization website, etc.)
An example Staff Acknowledgement Statement can be found at the end of this section.
Monitor Compliance
Like other organizational policy and practices, Confident Teen should be monitored over time to ensure compliance and effectiveness. Measurable goals and objectives can act as benchmarks for compliance and effectiveness.
Questions for your organization may include:
- Are all employees following the policy and procedures?
- Are monitoring plans developed in tandem with policy?
- Is there notable noncompliance among employees? If so, what steps are being taken to address the issue(s)?
Continuous Policy Monitoring
Healthcare organizations are in a continuous state of change. The Confident Teen Policy and Procedures will likely need to be modified over time, based on lessons learned. To stay current with regulations and best practices, monitor and update the policy on a regular basis. Most organizations have set parameters for policy review and the Confident Teen Policy should be incorporated into that review rotation. Routine monitoring will also ensure Confident Teen is effectively serving the needs of adolescents.
Policy Monitoring Tips
- In the early implementation phase, meet with key staff monthly to understand how the new policy is perceived by stakeholders (i.e., staff and clients). This phase is also an ideal time to gauge the level of stakeholder engagement.
- Make modifications to the policy based on lessons learned and document the progress of policy development. As you make modifications to the policy over time, reassess stakeholder engagement.
- As the policy becomes standard practice, you can monitor stakeholder perceptions and engagement less frequently. However, you should continue to appraise the policy environment over time.
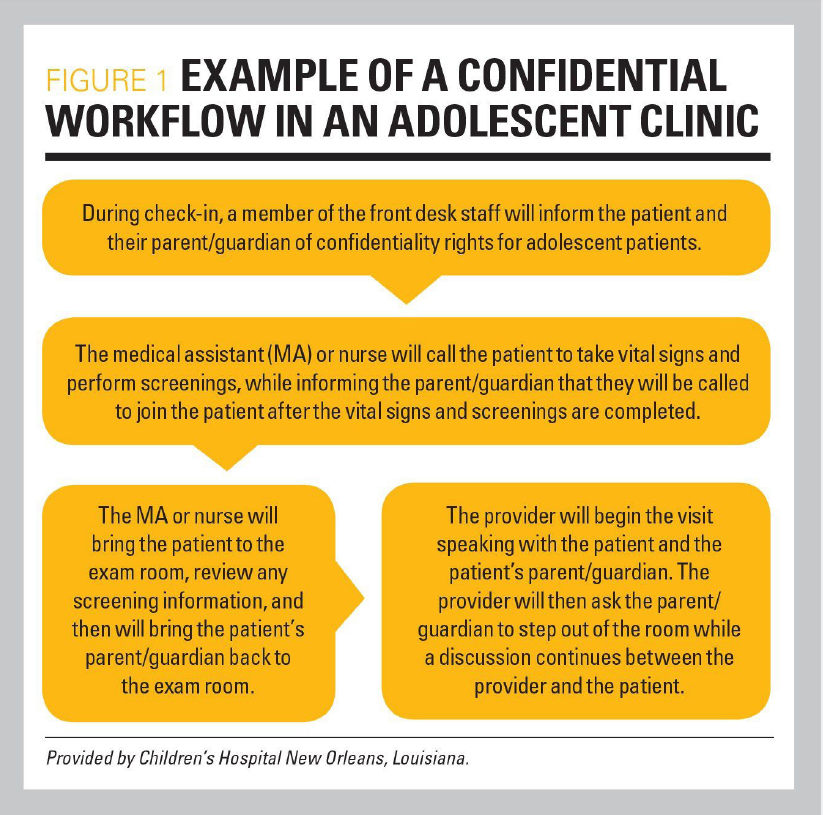
Clinic Workflow
When adopting the Confident Teen Policy, your organization will most likely have to modify existing clinic workflows and procedures for adolescent patient appointments. The following text describes the steps of the example workflow.
Click here to download a sample Confident Teen Clinic Workflow.
Before the Visit
Parents/guardians should receive an Appointment Reminder with information about the Confident Teen Policy when an appointment is scheduled for an adolescent (typically by the adolescent’s parents/ guardians).
The Appointment Reminder is the first communication with parents/guardians about your organization’s new approach to adolescent confidentiality. To facilitate buy-in among parents/guardians, your organization should share this information using several methods.
Click here to download a sample Appointment Reminder.
During the Visit
Patient Check-In
When the adolescent patient arrives for their appointment, they (and their parents/ guardians) will enter the waiting room and approach the front desk. The front desk staff will proceed with the patient check-in process, which typically involves completing clinic paperwork and consent forms.
During the check-in process, clinic staff will:
- Remind parents/guardians of the clinic policy regarding adolescent patients.
- Give parents/guardians the Policy Information for Parents and Guardians Handout, which explains the policy and the importance of confidentiality.
- Give the adolescent patient a Teen Clinic Policy Handout.
- Encourage adolescents to complete a consent form (if needed by your organization).
- Remind the adolescents that in most cases, parents still have the right to access information provided on all medical forms.
Click here to download Confident Teen Clinic Policy.
Click here to download Policy Information for Parents and Guardians.
Vital Check
Once check-in is complete, a provider (typically a nurse, clinical assistant, or medical assistant) will escort the adolescent into the exam area. At this time, parents/guardians will remain in the waiting room.
The provider will proceed with the adolescent’s vital check (e.g., measuring height, weight, blood pressure, etc.). During this time, the provider will give the adolescent a tablet or iPad, explain the purpose of the Total Teen Assessment, and ask them to complete it independently.
If your workflow allows for it, encourage the patient to browse adolescent-friendly health resources available in the exam area (e.g., physical posters and/or digital tools) while they wait for their primary care provider. If there are tear cards for services provided, be sure to tear off a few cards in advance so the patient won’t be the first person to remove an information card.
Click here to download Health Resources for Teens.
Confidential Appointment Time
When the primary care provider enters the exam room, they will begin a confidential one-on-one conversation with the patient following these steps:
- Introduce themselves and get to know the adolescent or re-establish an existing provider/patient relationship.
- Define confidentiality between an adolescent and provider. Be very clear about what would constitute breaking confidentiality.
- Discuss instances in which confidentiality may be breached (i.e., conditional confidentiality).
- Sample conversations between adolescent patients and providers can be found in the Communication Section.
Confidentiality between a provider and the patient means:
- Keeping information the patient shares private, unless it requires mandated reporting to appropriate authorities (e.g., if you suspect the patient is at risk of harming themself, harming someone else, or being harmed by someone)
- Not telling anyone about the patient’s visit or that they are a patient at your clinic
Providers must be cautious not to document confidential matters in EMR/EHR records to ensure that information is not accessible by parents/guardians through medical records.
Consent and Assent
To make confidential adolescent-provider time part of regular practice, we recommend organizations implement Confident Teen as an opt-out policy. This ensures adolescent patients have access to one-on-one time with their provider, unless they or their parents/guardians say otherwise (i.e., opt out of it). The information below provides context for consent and assent processes associated with the policy for adolescents and their parents/guardians.
Note: All states have different laws regarding minor access to confidential care and services. It is the responsibility of your organization to determine the best consent process based on state and local laws and governing bodies. Should your organization require parents/guardians to sign a consent form, a template is provided at the end of this section for you to use. If you are unsure, consult your legal counsel, healthcare administrators, or board of directors.
Parent/Guardian Consent
Communicating with parents/guardians about the policy and consent process is important. All healthcare organizations require parents/guardians consent for treatment. Your organization can include the Policy and Procedures in standard consent for treatment forms, because it is organizational policy and part of normal workflow.
Consider the following steps when modifying consent and assent processes within your clinic:
- Determine the appropriate consent process for parents/guardians within your organization and a process to opt out of the confidential time if needed.
- If your organization requires a formal consent form, see the Policy Consent Form for Parents/ Guardians example at the end of this section.
- Modify the Policy Consent Form for Parents/ Guardians to reflect state and local laws.
- Incorporate the Policy Consent Form for Parents/ Guardians into your organization’s patient intake process.
Click here to download Confident Teen Policy and Procedures Template.
Click here to download Policy Consent Form for Parents / Guardians.
Adolescent Assent
To fully embrace the adolescent-centered nature of Confident Teen, it is important to notify adolescents about the policy and provide them with a choice to participate. Although it is assumed adolescent patients will participate in the confidential sessions offered, your organization should let adolescents know they have the right to opt out of the service if they want their parent/guardian present for the entire appointment.
Adolescents may choose to opt-out if they:
- Are younger
- Are new to the practice/provider
- Are being offered the service for the first time (regardless of age)
- Have medical complexities
- Have complex psychosocial issues
Consider the following steps when modifying consent and assent processes within your clinic:
- Determine an appropriate assent process for adolescent patients in your clinic to ensure they are aware of the policy and given an opportunity to opt out if desired.
- Inform adolescents the service will be offered routinely to prevent them from misinterpreting the policy as coercive.
- Offer the service every visit.
Policy Notification
Informing Parents/Guardians
Timely communication between healthcare organizations and parents/guardians about the Confident Teen Policy assists with understanding and support. The Confident Teen Workflow calls for communication to inform teens’ parents/guardians about the policy and procedures before an appointment. Multiple approaches to this step are described below.
Appointment Reminders
One of the first opportunities to notify adolescents and their parents/guardians about the Confident Teen Policy is through appointment reminders. You may also want to provide a link to the policy on your clinic website(s) for clients to access beforehand. Example Appointment Reminders are provided at the end of this section. These examples may be used in conjunction with existing appointment reminders, to replace existing reminders, or as a model for future reminders.
Consider the following steps when modifying processes to include information about the policy:
- Incorporate policy information in appointment reminders, including a link to the organization’s policy.
- Ensure information about the policy is provided to the adolescent’s parents/ guardians prior to an appointment.
Note: The most important aspect of appointment reminders is the specific reference to Confident Teen Policy.
Parents/Guardians Handout
The Policy Information for Parents and Guardians Handout can be used to provide information about the policy’s importance, purpose, and how it works within the clinic space. The handout can be given to parents/ guardians during the check-in process, put on display at the front desk, posted online, and included in appointment reminders. An example Policy Information for Parents and Guardians Handout is provided at the end of this section.
Consider the following steps when modifying and incorporating the handout in your clinic:
- Make the handout available to view online, if possible.
- Link the handout in appointment reminders to parents/guardians.
- Provide parents/guardians with a physical, or digital copy of the handout via QR code, during the check-in process to review.
Click here to download Policy Information for Parents and Guardians.
Click here to download a sample Appointment Reminder.
Informing Adolescents
It is assumed adolescents will participate in the confidential sessions offered. However, your organization should make it clear to patients that they have the right to choose. You can share information about the policy with adolescent patients through the informational handout described below.
Teen Handouts
The one-page Confident Teen Policy Handout provides a brief explanation of the Confident Teen Policy, including the policy’s importance and how it works. The handout also lists topics adolescents may want to discuss during one-on-one time with their healthcare providers. The Confident Teen Policy Handout is provided at the end of this section.
Consider the following steps when modifying and incorporating the handout in your clinic:
- Make the handout available to view online, if possible.
- Link the handout in appointment reminders to adolescents.
- Give the handout to adolescents during the check-in process to review, or display
- QR code that links to the handout for them to scan.
Informing the Public
Consider ways to inform the public about the new clinic policies and procedures, the services provided, and the mission to increase access to adolescent-friendly healthcare services. Identify and inform key people within the community who serve as formal leaders or informal influencers for the community-at-large. It is especially important to consider individuals who serve or are adjacent to adolescents in your community, such as:
- Local leaders
- Other healthcare providers
- School officials
- School nurses
- Social service providers
- Faith leaders
- Business leaders
Methods to inform the public about this policy may include social media posts or press releases. Your organization may create a flyer to be shared with other local organizations. These efforts will assist with increasing awareness of your clinic’s adolescent-friendly policy and practices.
When creating materials and messages to inform the public, consider the following tips:
- Consult your media and marketing team.
- Make sure materials (including websites) are concise and accessible for a wide audience.
- Consult the American Disabilities Act (ADA) for recommendations on designing materials for accessibility (e.g., using large, bold fonts; using color combinations that are high in contrast and can be distinguished by those with visual impairments; etc.).
- Written content should be a Flesch-Kincaid Grade Level of 8 or below.
- Explore various free resources online to determine the Flesch-Kincaid Grade Level of written content (e.g., www.readable.com or www.online-utility.org).
See the 1) Flyer to Inform the Public (Template) and the 2) Flyer to Inform the Public (Example) provided at the end of this section for content and design ideas when creating informative materials.
Click here to download Confident Teen Clinic Policy.
Click here to download Flyer to Inform the Public (Template).
Click here to download Flyer to Inform the Public (Example).
Section in Review
This section, Coordination, focused on administrative practices essential to successful implementation of Confident Teen. The following list summarizes key information and tasks from this section:
- The policy and procedures should be modified to fit within an organization.
- All clinic staff should be informed of the policy, its purpose, and procedures.
- Confident Teen should be monitored over time to ensure compliance and effectiveness.
- When adopting the Confident Teen Policy, your organization should work collaboratively to modify existing clinic workflows and procedures for adolescent patient appointments.
- Organizations are responsible for determining the best consent and adolescent assent processes based on state and local laws and governing bodies.
- Organizations should notify adolescent patients and their parents/guardians about the Confident Teen Policy in a timely manner.
The above tasks and practices primarily occur within your organization. However, successful implementation of Confident Teen involves collaboration with other healthcare organizations, providers, and resources. Therefore, the next section, Collaboration, will focus on identifying and establishing a network of adolescentfriendly referral partners, a critical step to ensuring you meet all the needs of adolescent patients.
Collaboration
The second pillar of adolescent patient-centered care is Collaboration. Collaboration ensures organizations have an adolescent-friendly network of providers and resources. A key component of adolescent-friendly care is not only providing confidential services, but connecting patients to additional services (including those requiring internal or external referrals) in a timely manner.
Establish a Network of Adolescent-Friendly Referral Partners
Healthcare organizations should have an identified network of trusted providers to whom they can refer adolescents. Specifically, you will know which sexual and reproductive health and/or mental health providers can provide timely, high-quality, confidential services to your adolescent patients. It is crucial referrals for future services be made on the same day to reduce barriers to accessing follow-up services. The network may include referral partners who are in-network, out-of-network, and/or community-based service providers. Consider services both local and national in scope; local providers may offer in-person services, while providers in other geographic regions may provide telehealth services.
Additionally, you should ensure the providers you refer patients to offer adolescent-friendly services and will not shame, refuse, or dismiss adolescent needs. Clinics should periodically assess if their referral sites adhere to adolescent-friendly standards (refer back to Preparing Organizations to Implement for details about adolescent-friendly services and providers). Consideration of adolescent-friendly services is important to establishing rapport and trust between the provider and the adolescent.
At the end of this section are templates to use for developing your database of adolescent-friendly referral partners. This template serves as a starting point; it is not all-encompassing and should be adapted to meet your organization and community’s needs. Within the database, it is strongly recommended you develop three lists to distinguish:
- Sexual and reproductive health providers
- Mental health providers
- Other providers and resources
These lists are essential to providing multiple sources of support for adolescents’ encounters with the healthcare system. As the Total Teen Assessment is designed to identify SRH and MH needs, it is critical your organization take the time to establish a robust and well-rounded database of adolescent-friendly referral partners.
Click here to download Steps to Establish a Network of Adolescent-Friendly Partners.
Tips for Referral Best Practices
<- Have patients identify sources of support they are comfortable contacting as needed.
- Incorporate more than just referrals in your practice; provide patients with adolescent-friendly resources (both local and national) that provide reliable information based on the patients’ needs.
- For patients that have a referral within one month:
- Confirm they attended their appointment.
- If the patient did not attend the appointment, help them schedule a new one.
- For patients with referrals exceeding one month:
- Identify a staff member who can contact the patient every two weeks to check-in on the status of their referral appointment.
- For patients with more acute needs, consider scheduling regular check-ins (until they are able to see a specialist) to monitor symptoms and concerns. If symptoms appear to worsen, discuss options for more immediate treatment or intervention.
Click here to download a Sexual and Reproductive Healthcare Providers worksheet.
Click here to download a Mental Health Providers worksheet.
Additional Resources for Adolescents
<It is important to inventory both local and national scale resources that provide reliable information for teens; include local non-profits, businesses, and social service organizations.
Depending on the adolescent’s needs, not every adolescent will require or be ready for additional healthcare services. In some cases, they will need more information to be comfortable accessing specialty care, or they may need more time to research options and determine their choice for next steps. Empowering adolescents to take ownership of their health will ultimately contribute to improved access to care.
Section in Review
Referring patients to adolescent-friendly healthcare organizations and providers for specialized care can facilitate access to care. This section focused on establishing an adolescent-friendly network of referral partners. The following list summarizes key information and tasks from this section:
- A collaborative, interdisciplinary approach to adolescent patient-centered care can ensure adolescents’ healthcare needs are met.
- Healthcare organizations should identify and establish a network of adolescent-friendly referral partners.
- Timeliness is essential. When establishing network referral partners, processes should be put in place to ensure patient referrals can be made on the same day as an adolescent patient’s appointment.
- It is important to know where to find reliable adolescent-friendly resources, as well as to know who the key stakeholders are within your community and how to engage them.
- In addition to providers for direct referrals, take inventory of both local and national scale resources that provide reliable information for adolescents.
Organizations can ensure adolescent healthcare needs are met by establishing an adolescent-friendly referral network. The next section, Communication, will focus on provider-patient communication, which is a critical aspect of adolescents’ access to and experiences with healthcare.
Communication
The third pillar of adolescent patient-centered care is communication, which is the interpersonal communication between healthcare providers, patients, and various stakeholders. Communication about the Confident Teen Policy should begin before healthcare appointments and continue throughout the services the teen receives.
Information for Providers
The Confident Teen Policy and procedures provide adolescents the opportunity to have oneon- one time with their healthcare provider(s). The purpose of this time is to allow adolescents an opportunity to discuss questions and concerns with their providers. This individual time will help promote positive patient-provider communication and increase patient comfort in talking with healthcare providers about sensitive topics.
As a healthcare provider, assure adolescent patients their conversations with you will remain confidential. You should discuss confidentiality policies with them, including conditions under which you cannot uphold confidentiality. It is crucial you clearly explain to adolescent patients what information cannot be kept confidential and warrants mandatory reporting. It is critical that you be very clear and concrete about what constitutes mandatory reporting, and what will remain confidential. You do not want patients worried that you will report minor things (e.g., smoking a cigarette) and then withhold information from you.
Once the adolescent is finished talking about confidential matters with you, their parents/guardians may join them for the rest of the appointment. It is your responsibility to ensure confidential topics discussed during one-on-one time are not discussed in front of parents/guardians, unless agreed upon with the adolescent patient.
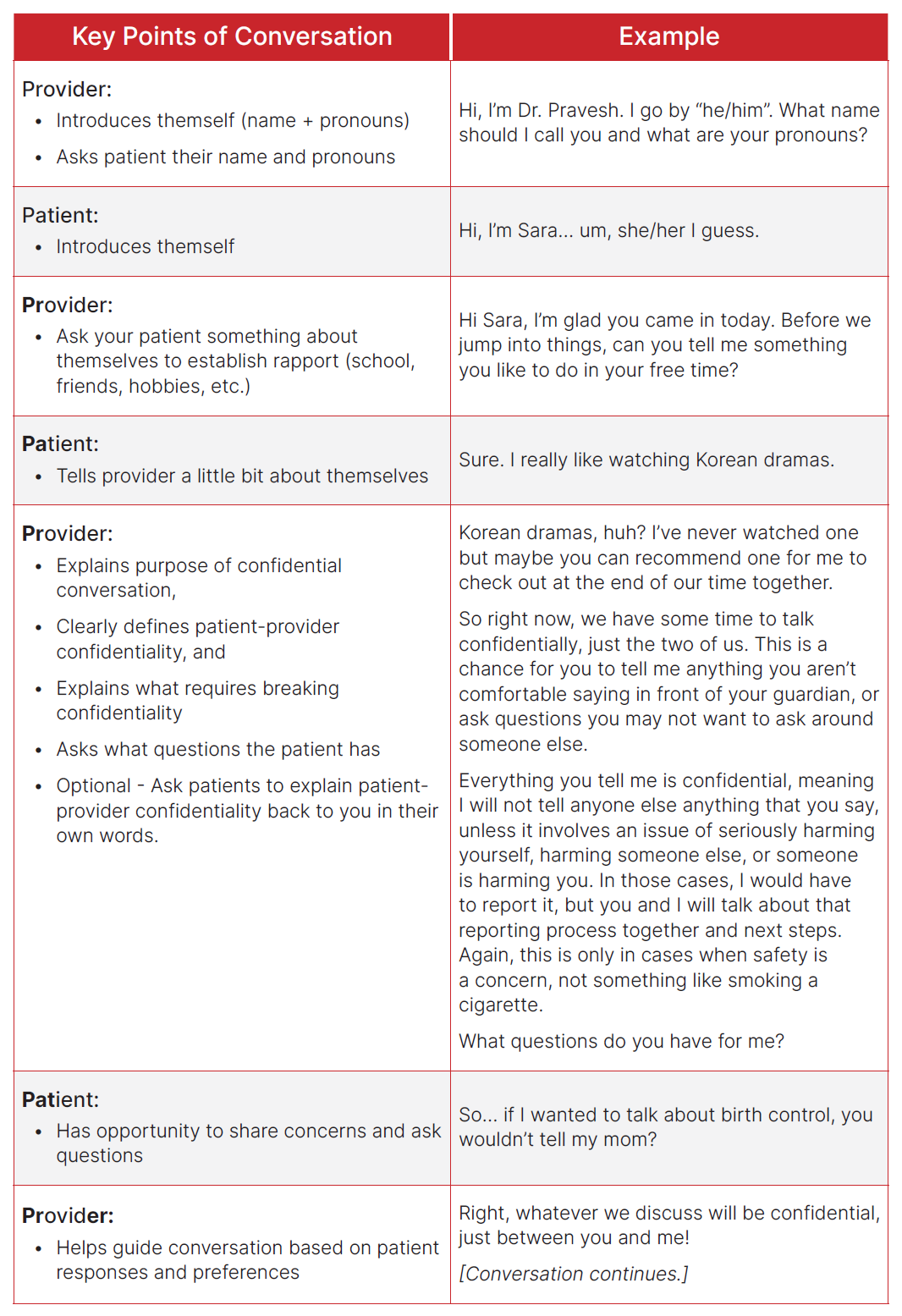
Talking with Adolescent Patients
Conversations with adolescent patients will vary based on multiple factors, including but not limited to: comfort, knowledge and awareness, culture, communication styles, experiences, etc. However, every conversation should include the key points in the table on the following page.
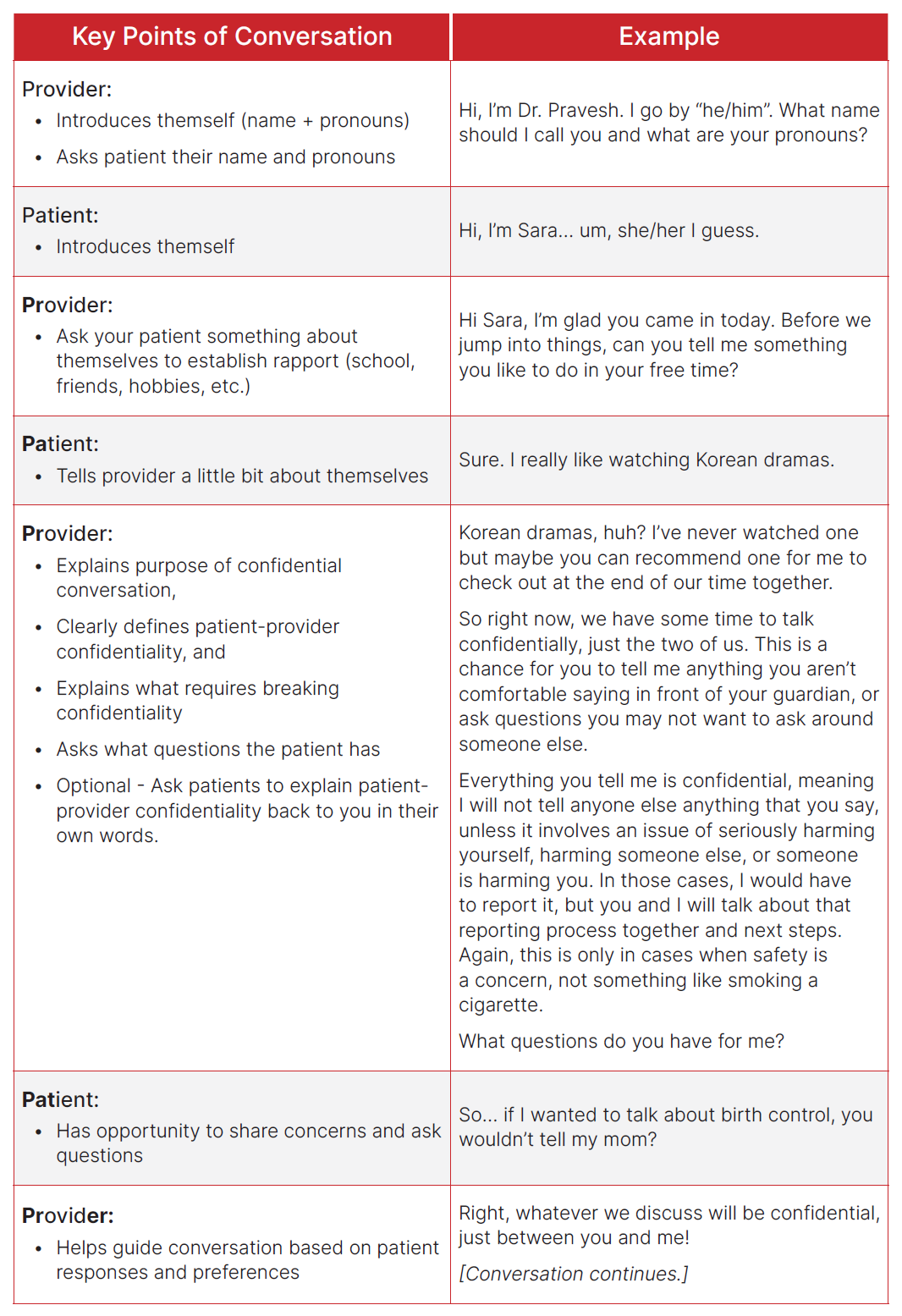
First, healthcare providers should introduce themselves and allow adolescents to do the same. When working with adolescents, providers need to be prepared to start the conversation. This includes asking the patients about themselves; start with “small talk” to establish rapport before “big talk.”
Next, providers should thank the patient for coming in, explain confidentiality and the purpose of confidential conversations. During this time, the provider should clearly define patient-provider confidentiality, and explain what requires breaking confidentiality. Be very concrete about what constitutes mandatory reporting so that patients do not withhold information out of fear of reporting. Consider asking patients to repeat back to you what they understand confidentiality to be, and what will be kept confidential. This is the time to clarify any misunderstandings of patient-provider confidentiality, and then ask the patient what questions they have.
Note: Providers should not chart confidential conversations in EMR/EHR files, unless there is a confidential field that is only accessible to providers (e.g., there is no way for parents/guardians to see the information through medical records).
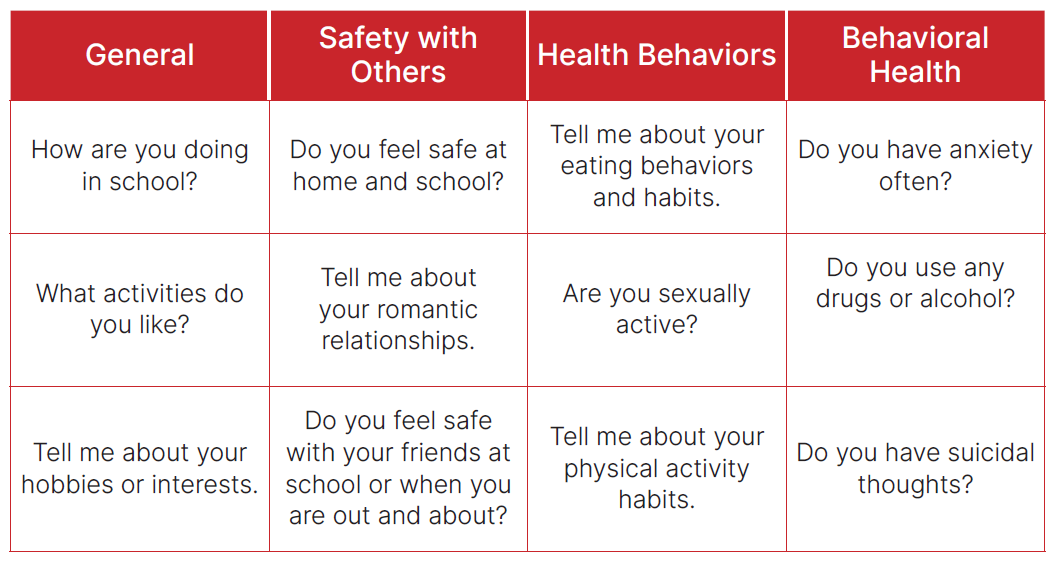
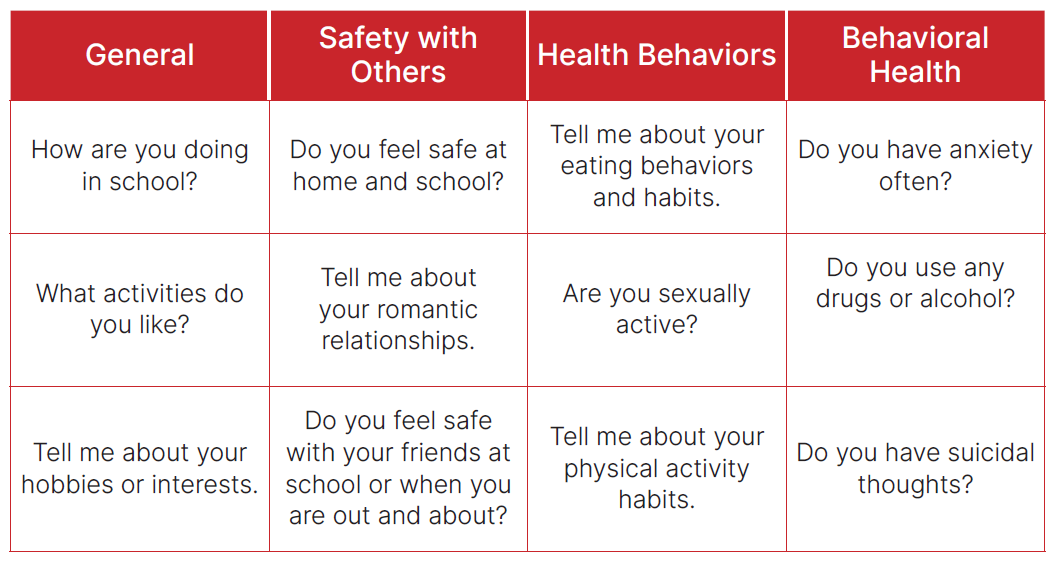
Throughout the appointment, providers may ask teens a range of questions to learn more about them, their health habits, and potential needs. Below is a list of potential questions to guide the confidential conversations. Both open-ended and closed-ended questions are included. Still, some teens will be uncomfortable talking with an adult or professional about sensitive topics.
Tips for Talking with Adolescent Patients
- Use age-appropriate language, and recognize the developmental differences in adolescent patients (compared to children or younger patients).
- Ask patients to repeat information back to you in their own words to ensure their understanding.
- Be aware of body language; avoid expressing shock from a patient’s response.
- Maintain a tone of mutual respect and understanding; take care to not sound condescending.
- Reassure patients and make them feel in control of what they are going through; recognize the strengths in their stories and experiences.
- Validate the patient; listen to them and make it a two-way discussion rather than a checklist of questions and answers.
Remember: This confidential conversation may be the only time for adolescents to talk with you or other providers about potentially sensitive topics. You may also need to talk with adolescents about follow-up services, where to go for support, or next steps in their care.
Sample Conversations for Providers
The CHAI teen advisory group (TAG) developed a set of sample conversations to provide examples of how these conversations may go. Each conversation will vary, therefore multiple examples are provided at the end of this section.
Within the sample conversations, you may notice:
- Patients of different ages and life experiences
- Various questions used to generate conversation and ask the patients about themselves
- Questions about who they go to for support
- Conversations discussing additional details about certain topics
- Sample phrases to assure patients their conversations will remain confidential
Note: These are not perfect examples of confidential conversations. Rather, they are a tool for you to see samples of language and responses used by adolescents.
Click here to download Sample Provider Scripts.
Discussing Sensitive Topics
Discussing private or sensitive topics (e.g., sexual health or mental health) can be stressful and uncomfortable for adolescents. They may be unprepared for the private meeting time with the provider or forget their questions. Providing a list of topics can help put the teen at ease while fostering an opportunity to discuss such health matters. Consider using the Discussing Sensitive Topics handout (found at the end of this section) as a way for teens to identify and communicate their interests and needs with you. It should be given to the teen during their vital check to identify topics and questions to discuss with the provider during their one-on-one time.
Click here to download Discussing Sensitive Topics.
Section in Review
Timely and appropriate communication throughout the healthcare experience is critical. This section focused on communication between providers and adolescent patients. The following list summarizes key information and tasks from this section:
- Adolescent patient-centered care involves interpersonal communication between providers, patients, and various stakeholders.
- Adolescent patients may be unprepared for confidential conversations or forget their questions. Providing a list of health topics can help put patients at ease and facilitate provider-patient discussions.
- Assuring adolescent patients that their conversations with providers are confidential can encourage discussion about sensitive health topics.
- Providers should discuss conditional confidentiality with their adolescent patients. It is especially important to describe circumstances where confidentiality cannot be upheld.
- Consider initiating provider-patient conversations with “small talk” before “big talk.”
The following section focuses on providing confidential care in an efficient manner for adolescent patients.
Care
The fourth and final pillar of adolescent patient-centered care is care, which ensures providing quality confidential care to adolescent patients. The care they receive is a continuum - it begins from the moment patients enter the clinic and continues after they leave through follow-up services, future appointments, and even additional points of contact between patients and providers such as e-messages and phone calls.
Confidential Care
Adolescents should have access to confidential healthcare services. It allows them to build their skill set for navigating the healthcare environment and begin making informed decisions regarding their health. However, it is imperative that healthcare providers understand what constitutes confidential care.
Confidentiality means that unless a patient gives consent, you will not:
- Tell anyone about their visit.
- Tell anyone that they are a patient at your clinic.
- Pass on any of their personal information to anyone.
Topics discussed during the confidential conversation should not be shared with parents/ guardians unless approved by the adolescent patient. As HIPAA regulations generally allow a parent/guardian to have access to medical records for their children under the age of 18, it is imperative that providers document any details regarding confidential conversations in a secure manner that is not accessible to parents/guardians. It is the responsibility of each organization to determine the best process for providers to take notes on confidential conversations in a manner that is secure and separate from appointment information accessible to parents/guardians. This will be dependent upon state and local laws, along with electronic medical record (EMR) functionality and capabilities, and organizational policies and practices for documenting patient notes.
Confidential conversations may be disclosed to parents/guardians or local authorities if the patient is in immediate danger to themselves or another person. In such cases, providers should discuss next steps for informing parents/guardians with the teen, as well as any state reporting that is required. Confidentiality is conditional, and should be clearly defined for the patients, particularly instances that warrant mandatory reporting (e.g., when there is concern for the safety of a patient or others).
If the confidential conversation leads to a referral or follow-up appointment for additional care and services, the healthcare provider and teen should discuss together, how best to disclose the need for the upcoming appointment. In such cases, it is important that the teen and provider discuss this together, so the teen still feels in control and part of the decision-making process.
Section in Review
Adolescent patient-centered care ensures adolescents receive confidential care. This section focused on ensuring and providing confidentiality in adolescent patient-centered care. The following list summarizes key information and tasks from this section:
- Confidential care means not divulging details about a patient or a patient’s appointment with anyone, including but not limited to the patient’s parents/ guardians and other health professionals.
- Any details documented by providers should be done in a secure manner to ensure providers document notes are separate from medical records accessible to parents/guardians.
- Confidentiality is conditional; certain information may be disclosed with others and such cases should be clearly explained to adolescent patients.
- Providers should involve adolescent patients in decision-making as often as possible.
First, healthcare providers should introduce themselves and allow adolescents to do the same. When working with adolescents, providers need to be prepared to start the conversation. This includes asking the patients about themselves; start with “small talk” to establish rapport before “big talk.”
Next, providers should thank the patient for coming in, explain confidentiality and the purpose of confidential conversations. During this time, the provider should clearly define patient-provider confidentiality, and explain what requires breaking confidentiality. Be very concrete about what constitutes mandatory reporting so that patients do not withhold information out of fear of reporting. Consider asking patients to repeat back to you what they understand confidentiality to be, and what will be kept confidential. This is the time to clarify any misunderstandings of patient-provider confidentiality, and then ask the patient what questions they have.
Note: Providers should not chart confidential conversations in EMR/EHR files, unless there is a confidential field that is only accessible to providers (e.g., there is no way for parents/guardians to see the information through medical records).
Throughout the appointment, providers may ask teens a range of questions to learn more about them, their health habits, and potential needs. Below is a list of potential questions to guide the confidential conversations. Both open-ended and closed-ended questions are included. Still, some teens will be uncomfortable talking with an adult or professional about sensitive topics.
Tips for Talking with Adolescent Patients
- Use age-appropriate language, and recognize the developmental differences in adolescent patients (compared to children or younger patients).
- Ask patients to repeat information back to you in their own words to ensure their understanding.
- Be aware of body language; avoid expressing shock from a patient’s response.
- Maintain a tone of mutual respect and understanding; take care to not sound condescending.
- Reassure patients and make them feel in control of what they are going through; recognize the strengths in their stories and experiences.
- Validate the patient; listen to them and make it a two-way discussion rather than a checklist of questions and answers.
Remember: This confidential conversation may be the only time for adolescents to talk with you or other providers about potentially sensitive topics. You may also need to talk with adolescents about follow-up services, where to go for support, or next steps in their care.
Sample Conversations for Providers
The CHAI teen advisory group (TAG) developed a set of sample conversations to provide examples of how these conversations may go. Each conversation will vary, therefore multiple examples are provided at the end of this section.
Within the sample conversations, you may notice:
- Patients of different ages and life experiences
- Various questions used to generate conversation and ask the patients about themselves
- Questions about who they go to for support
- Conversations discussing additional details about certain topics
- Sample phrases to assure patients their conversations will remain confidential
Note: These are not perfect examples of confidential conversations. Rather, they are a tool for you to see samples of language and responses used by adolescents.
Click here to download Sample Provider Scripts.
Discussing Sensitive Topics
Discussing private or sensitive topics (e.g., sexual health or mental health) can be stressful and uncomfortable for adolescents. They may be unprepared for the private meeting time with the provider or forget their questions. Providing a list of topics can help put the teen at ease while fostering an opportunity to discuss such health matters. Consider using the Discussing Sensitive Topics handout (found at the end of this section) as a way for teens to identify and communicate their interests and needs with you. It should be given to the teen during their vital check to identify topics and questions to discuss with the provider during their one-on-one time.
Click here to download Discussing Sensitive Topics.
Section in Review
Timely and appropriate communication throughout the healthcare experience is critical. This section focused on communication between providers and adolescent patients. The following list summarizes key information and tasks from this section:
- Adolescent patient-centered care involves interpersonal communication between providers, patients, and various stakeholders.
- Adolescent patients may be unprepared for confidential conversations or forget their questions. Providing a list of health topics can help put patients at ease and facilitate provider-patient discussions.
- Assuring adolescent patients that their conversations with providers are confidential can encourage discussion about sensitive health topics.
- Providers should discuss conditional confidentiality with their adolescent patients. It is especially important to describe circumstances where confidentiality cannot be upheld.
- Consider initiating provider-patient conversations with “small talk” before “big talk.”
The following section focuses on providing confidential care in an efficient manner for adolescent patients.
The second pillar of adolescent patient-centered care is Collaboration. Collaboration ensures organizations have an adolescent-friendly network of providers and resources. A key component of adolescent-friendly care is not only providing confidential services, but connecting patients to additional services (including those requiring internal or external referrals) in a timely manner.
Establish a Network of Adolescent-Friendly Referral Partners
Healthcare organizations should have an identified network of trusted providers to whom they can refer adolescents. Specifically, you will know which sexual and reproductive health and/or mental health providers can provide timely, high-quality, confidential services to your adolescent patients. It is crucial referrals for future services be made on the same day to reduce barriers to accessing follow-up services. The network may include referral partners who are in-network, out-of-network, and/or community-based service providers. Consider services both local and national in scope; local providers may offer in-person services, while providers in other geographic regions may provide telehealth services.
Additionally, you should ensure the providers you refer patients to offer adolescent-friendly services and will not shame, refuse, or dismiss adolescent needs. Clinics should periodically assess if their referral sites adhere to adolescent-friendly standards (refer back to Preparing Organizations to Implement for details about adolescent-friendly services and providers). Consideration of adolescent-friendly services is important to establishing rapport and trust between the provider and the adolescent.
At the end of this section are templates to use for developing your database of adolescent-friendly referral partners. This template serves as a starting point; it is not all-encompassing and should be adapted to meet your organization and community’s needs. Within the database, it is strongly recommended you develop three lists to distinguish:
Sexual and reproductive health providers
Mental health providers
Other providers and resources
These lists are essential to providing multiple sources of support for adolescents’ encounters with the healthcare system. As the Total Teen Assessment is designed to identify SRH and MH needs, it is critical your organization take the time to establish a robust and well-rounded database of adolescent-friendly referral partners.
Click here to download Steps to Establish a Network of Adolescent-Friendly Partners.
Tips for Referral Best Practices< Have patients identify sources of support they are comfortable contacting as needed. Incorporate more than just referrals in your practice; provide patients with adolescent-friendly resources (both local and national) that provide reliable information based on the patients’ needs. For patients that have a referral within one month: Confirm they attended their appointment. If the patient did not attend the appointment, help them schedule a new one. For patients with referrals exceeding one month: Identify a staff member who can contact the patient every two weeks to check-in on the status of their referral appointment. For patients with more acute needs, consider scheduling regular check-ins (until they are able to see a specialist) to monitor symptoms and concerns. If symptoms appear to worsen, discuss options for more immediate treatment or intervention. Click here to download a Sexual and Reproductive Healthcare Providers worksheet. Click here to download a Mental Health Providers worksheet. Additional Resources for Adolescents< It is important to inventory both local and national scale resources that provide reliable information for teens; include local non-profits, businesses, and social service organizations. Depending on the adolescent’s needs, not every adolescent will require or be ready for additional healthcare services. In some cases, they will need more information to be comfortable accessing specialty care, or they may need more time to research options and determine their choice for next steps. Empowering adolescents to take ownership of their health will ultimately contribute to improved access to care. Section in Review Referring patients to adolescent-friendly healthcare organizations and providers for specialized care can facilitate access to care. This section focused on establishing an adolescent-friendly network of referral partners. The following list summarizes key information and tasks from this section: A collaborative, interdisciplinary approach to adolescent patient-centered care can ensure adolescents’ healthcare needs are met. Healthcare organizations should identify and establish a network of adolescent-friendly referral partners. Timeliness is essential. When establishing network referral partners, processes should be put in place to ensure patient referrals can be made on the same day as an adolescent patient’s appointment. It is important to know where to find reliable adolescent-friendly resources, as well as to know who the key stakeholders are within your community and how to engage them. In addition to providers for direct referrals, take inventory of both local and national scale resources that provide reliable information for adolescents. Organizations can ensure adolescent healthcare needs are met by establishing an adolescent-friendly referral network. The next section, Communication, will focus on provider-patient communication, which is a critical aspect of adolescents’ access to and experiences with healthcare.\n\n[/cs_content_seo][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][cs_element_section _id="40" ][cs_element_layout_row _id="41" ][cs_element_layout_column _id="42" ][cs_element_layout_div _id="43" ][cs_element_text _id="44" ][cs_content_seo]\n\n[/cs_content_seo][/cs_element_layout_div][cs_element_text _id="45" ][cs_content_seo]Communication The third pillar of adolescent patient-centered care is communication, which is the interpersonal communication between healthcare providers, patients, and various stakeholders. Communication about the Confident Teen Policy should begin before healthcare appointments and continue throughout the services the teen receives. Information for Providers The Confident Teen Policy and procedures provide adolescents the opportunity to have oneon- one time with their healthcare provider(s). The purpose of this time is to allow adolescents an opportunity to discuss questions and concerns with their providers. This individual time will help promote positive patient-provider communication and increase patient comfort in talking with healthcare providers about sensitive topics. As a healthcare provider, assure adolescent patients their conversations with you will remain confidential. You should discuss confidentiality policies with them, including conditions under which you cannot uphold confidentiality. It is crucial you clearly explain to adolescent patients what information cannot be kept confidential and warrants mandatory reporting. It is critical that you be very clear and concrete about what constitutes mandatory reporting, and what will remain confidential. You do not want patients worried that you will report minor things (e.g., smoking a cigarette) and then withhold information from you. Once the adolescent is finished talking about confidential matters with you, their parents/guardians may join them for the rest of the appointment. It is your responsibility to ensure confidential topics discussed during one-on-one time are not discussed in front of parents/guardians, unless agreed upon with the adolescent patient. Talking with Adolescent Patients Conversations with adolescent patients will vary based on multiple factors, including but not limited to: comfort, knowledge and awareness, culture, communication styles, experiences, etc. However, every conversation should include the key points in the table on the following page.\n\n[/cs_content_seo][cs_element_image _id="46" ][cs_element_text _id="47" ][cs_content_seo]First, healthcare providers should introduce themselves and allow adolescents to do the same. When working with adolescents, providers need to be prepared to start the conversation. This includes asking the patients about themselves; start with “small talk” to establish rapport before “big talk.” Next, providers should thank the patient for coming in, explain confidentiality and the purpose of confidential conversations. During this time, the provider should clearly define patient-provider confidentiality, and explain what requires breaking confidentiality. Be very concrete about what constitutes mandatory reporting so that patients do not withhold information out of fear of reporting. Consider asking patients to repeat back to you what they understand confidentiality to be, and what will be kept confidential. This is the time to clarify any misunderstandings of patient-provider confidentiality, and then ask the patient what questions they have. Note: Providers should not chart confidential conversations in EMR/EHR files, unless there is a confidential field that is only accessible to providers (e.g., there is no way for parents/guardians to see the information through medical records). Throughout the appointment, providers may ask teens a range of questions to learn more about them, their health habits, and potential needs. Below is a list of potential questions to guide the confidential conversations. Both open-ended and closed-ended questions are included. Still, some teens will be uncomfortable talking with an adult or professional about sensitive topics.\n\n[/cs_content_seo][cs_element_image _id="48" ][cs_element_text _id="49" ][cs_content_seo]Tips for Talking with Adolescent Patients Use age-appropriate language, and recognize the developmental differences in adolescent patients (compared to children or younger patients). Ask patients to repeat information back to you in their own words to ensure their understanding. Be aware of body language; avoid expressing shock from a patient’s response. Maintain a tone of mutual respect and understanding; take care to not sound condescending. Reassure patients and make them feel in control of what they are going through; recognize the strengths in their stories and experiences. Validate the patient; listen to them and make it a two-way discussion rather than a checklist of questions and answers. Remember: This confidential conversation may be the only time for adolescents to talk with you or other providers about potentially sensitive topics. You may also need to talk with adolescents about follow-up services, where to go for support, or next steps in their care. Sample Conversations for Providers The CHAI teen advisory group (TAG) developed a set of sample conversations to provide examples of how these conversations may go. Each conversation will vary, therefore multiple examples are provided at the end of this section. Within the sample conversations, you may notice: Patients of different ages and life experiences Various questions used to generate conversation and ask the patients about themselves Questions about who they go to for support Conversations discussing additional details about certain topics Sample phrases to assure patients their conversations will remain confidential Note: These are not perfect examples of confidential conversations. Rather, they are a tool for you to see samples of language and responses used by adolescents. Click here to download Sample Provider Scripts. Discussing Sensitive Topics Discussing private or sensitive topics (e.g., sexual health or mental health) can be stressful and uncomfortable for adolescents. They may be unprepared for the private meeting time with the provider or forget their questions. Providing a list of topics can help put the teen at ease while fostering an opportunity to discuss such health matters. Consider using the Discussing Sensitive Topics handout (found at the end of this section) as a way for teens to identify and communicate their interests and needs with you. It should be given to the teen during their vital check to identify topics and questions to discuss with the provider during their one-on-one time. Click here to download Discussing Sensitive Topics. Section in Review Timely and appropriate communication throughout the healthcare experience is critical. This section focused on communication between providers and adolescent patients. The following list summarizes key information and tasks from this section: Adolescent patient-centered care involves interpersonal communication between providers, patients, and various stakeholders. Adolescent patients may be unprepared for confidential conversations or forget their questions. Providing a list of health topics can help put patients at ease and facilitate provider-patient discussions. Assuring adolescent patients that their conversations with providers are confidential can encourage discussion about sensitive health topics. Providers should discuss conditional confidentiality with their adolescent patients. It is especially important to describe circumstances where confidentiality cannot be upheld. Consider initiating provider-patient conversations with “small talk” before “big talk.” The following section focuses on providing confidential care in an efficient manner for adolescent patients.\n\n[/cs_content_seo][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][cs_element_section _id="50" ][cs_element_layout_row _id="51" ][cs_element_layout_column _id="52" ][cs_element_layout_div _id="53" ][cs_element_text _id="54" ][cs_content_seo]\n\n[/cs_content_seo][/cs_element_layout_div][cs_element_text _id="55" ][cs_content_seo]Care The fourth and final pillar of adolescent patient-centered care is care, which ensures providing quality confidential care to adolescent patients. The care they receive is a continuum - it begins from the moment patients enter the clinic and continues after they leave through follow-up services, future appointments, and even additional points of contact between patients and providers such as e-messages and phone calls. Confidential Care Adolescents should have access to confidential healthcare services. It allows them to build their skill set for navigating the healthcare environment and begin making informed decisions regarding their health. However, it is imperative that healthcare providers understand what constitutes confidential care. Confidentiality means that unless a patient gives consent, you will not: Tell anyone about their visit. Tell anyone that they are a patient at your clinic. Pass on any of their personal information to anyone. Topics discussed during the confidential conversation should not be shared with parents/ guardians unless approved by the adolescent patient. As HIPAA regulations generally allow a parent/guardian to have access to medical records for their children under the age of 18, it is imperative that providers document any details regarding confidential conversations in a secure manner that is not accessible to parents/guardians. It is the responsibility of each organization to determine the best process for providers to take notes on confidential conversations in a manner that is secure and separate from appointment information accessible to parents/guardians. This will be dependent upon state and local laws, along with electronic medical record (EMR) functionality and capabilities, and organizational policies and practices for documenting patient notes. Confidential conversations may be disclosed to parents/guardians or local authorities if the patient is in immediate danger to themselves or another person. In such cases, providers should discuss next steps for informing parents/guardians with the teen, as well as any state reporting that is required. Confidentiality is conditional, and should be clearly defined for the patients, particularly instances that warrant mandatory reporting (e.g., when there is concern for the safety of a patient or others). If the confidential conversation leads to a referral or follow-up appointment for additional care and services, the healthcare provider and teen should discuss together, how best to disclose the need for the upcoming appointment. In such cases, it is important that the teen and provider discuss this together, so the teen still feels in control and part of the decision-making process. Section in Review Adolescent patient-centered care ensures adolescents receive confidential care. This section focused on ensuring and providing confidentiality in adolescent patient-centered care. The following list summarizes key information and tasks from this section: Confidential care means not divulging details about a patient or a patient’s appointment with anyone, including but not limited to the patient’s parents/ guardians and other health professionals. Any details documented by providers should be done in a secure manner to ensure providers document notes are separate from medical records accessible to parents/guardians. Confidentiality is conditional; certain information may be disclosed with others and such cases should be clearly explained to adolescent patients. Providers should involve adolescent patients in decision-making as often as possible. \n\n[/cs_content_seo][cs_element_image _id="56" ][cs_element_text _id="57" ][cs_content_seo]First, healthcare providers should introduce themselves and allow adolescents to do the same. When working with adolescents, providers need to be prepared to start the conversation. This includes asking the patients about themselves; start with “small talk” to establish rapport before “big talk.” Next, providers should thank the patient for coming in, explain confidentiality and the purpose of confidential conversations. During this time, the provider should clearly define patient-provider confidentiality, and explain what requires breaking confidentiality. Be very concrete about what constitutes mandatory reporting so that patients do not withhold information out of fear of reporting. Consider asking patients to repeat back to you what they understand confidentiality to be, and what will be kept confidential. This is the time to clarify any misunderstandings of patient-provider confidentiality, and then ask the patient what questions they have. Note: Providers should not chart confidential conversations in EMR/EHR files, unless there is a confidential field that is only accessible to providers (e.g., there is no way for parents/guardians to see the information through medical records). Throughout the appointment, providers may ask teens a range of questions to learn more about them, their health habits, and potential needs. Below is a list of potential questions to guide the confidential conversations. Both open-ended and closed-ended questions are included. Still, some teens will be uncomfortable talking with an adult or professional about sensitive topics.\n\n[/cs_content_seo][cs_element_image _id="58" ][cs_element_text _id="59" ][cs_content_seo]Tips for Talking with Adolescent Patients Use age-appropriate language, and recognize the developmental differences in adolescent patients (compared to children or younger patients). Ask patients to repeat information back to you in their own words to ensure their understanding. Be aware of body language; avoid expressing shock from a patient’s response. Maintain a tone of mutual respect and understanding; take care to not sound condescending. Reassure patients and make them feel in control of what they are going through; recognize the strengths in their stories and experiences. Validate the patient; listen to them and make it a two-way discussion rather than a checklist of questions and answers. Remember: This confidential conversation may be the only time for adolescents to talk with you or other providers about potentially sensitive topics. You may also need to talk with adolescents about follow-up services, where to go for support, or next steps in their care. Sample Conversations for Providers The CHAI teen advisory group (TAG) developed a set of sample conversations to provide examples of how these conversations may go. Each conversation will vary, therefore multiple examples are provided at the end of this section. Within the sample conversations, you may notice: Patients of different ages and life experiences Various questions used to generate conversation and ask the patients about themselves Questions about who they go to for support Conversations discussing additional details about certain topics Sample phrases to assure patients their conversations will remain confidential Note: These are not perfect examples of confidential conversations. Rather, they are a tool for you to see samples of language and responses used by adolescents. Click here to download Sample Provider Scripts. Discussing Sensitive Topics Discussing private or sensitive topics (e.g., sexual health or mental health) can be stressful and uncomfortable for adolescents. They may be unprepared for the private meeting time with the provider or forget their questions. Providing a list of topics can help put the teen at ease while fostering an opportunity to discuss such health matters. Consider using the Discussing Sensitive Topics handout (found at the end of this section) as a way for teens to identify and communicate their interests and needs with you. It should be given to the teen during their vital check to identify topics and questions to discuss with the provider during their one-on-one time. Click here to download Discussing Sensitive Topics. Section in Review Timely and appropriate communication throughout the healthcare experience is critical. This section focused on communication between providers and adolescent patients. The following list summarizes key information and tasks from this section: Adolescent patient-centered care involves interpersonal communication between providers, patients, and various stakeholders. Adolescent patients may be unprepared for confidential conversations or forget their questions. Providing a list of health topics can help put patients at ease and facilitate provider-patient discussions. Assuring adolescent patients that their conversations with providers are confidential can encourage discussion about sensitive health topics. Providers should discuss conditional confidentiality with their adolescent patients. It is especially important to describe circumstances where confidentiality cannot be upheld. Consider initiating provider-patient conversations with “small talk” before “big talk.” The following section focuses on providing confidential care in an efficient manner for adolescent patients.\n\n[/cs_content_seo][/cs_element_layout_column][/cs_element_layout_row][/cs_element_section][/cs_content]

